Epilepsy is a chronic neurological condition that affects brain function and manifests through recurrent epileptic seizures. It is one of the oldest neurological diseases known to medicine, yet it is still surrounded by misinformation and stigma. Understanding epilepsy is essential to reduce prejudice, identify symptoms early, and provide appropriate treatment.
In this text, we will explain what epilepsy is, its possible causes, types of seizures, treatment options, and debunk some of the most common myths about the condition.
What is epilepsy?
Epilepsy is characterized by abnormal electrical discharges in the brain, which cause short seizures. For a condition to be diagnosed as epilepsy, the patient must have had two or more unprovoked seizures — that is, not caused by high fever, alcohol withdrawal, or recent trauma.
These seizures can present in different ways — some are obvious, involving convulsions and loss of consciousness, while others are more subtle, such as lapses in attention or involuntary repetitive movements.
Causes of epilepsy
Epilepsy can have different origins, and in about half of the cases, the cause is unknown (idiopathic epilepsy). Known causes include:
Brain injuries: such as traumatic brain injury, tumors, or strokes.
Neurological infections: like meningitis, encephalitis, or neurocysticercosis.
Congenital malformations: abnormalities in brain development during the fetal stage.
Genetic alterations: some forms of epilepsy have a hereditary origin.
Metabolic disorders: such as hypoglycemia or electrolyte imbalances.
Birth complications: lack of oxygen to the brain may cause damage.
Types of epileptic seizures
Seizures are divided into two main groups: focal (partial) and generalized.
Focal seizures
These occur when abnormal electrical activity is limited to a specific area of the brain. They can be:
Simple: the person remains conscious but may have motor, sensory, or emotional changes.
Complex: consciousness is altered; the person may appear confused or perform automatic movements (like chewing or fidgeting).
Generalized seizures
These affect both hemispheres of the brain from the onset and usually impair consciousness. Examples:
Tonic-clonic seizure (convulsive): loss of consciousness, muscle stiffness followed by spasms and jerky movements. This is the most commonly recognized type.
Absence seizure: more common in children, characterized by brief lapses in awareness, with a blank stare or repeated blinking.
Myoclonic, tonic, or atonic seizures: involve sudden jerks, rigidity, or a sudden loss of muscle tone.
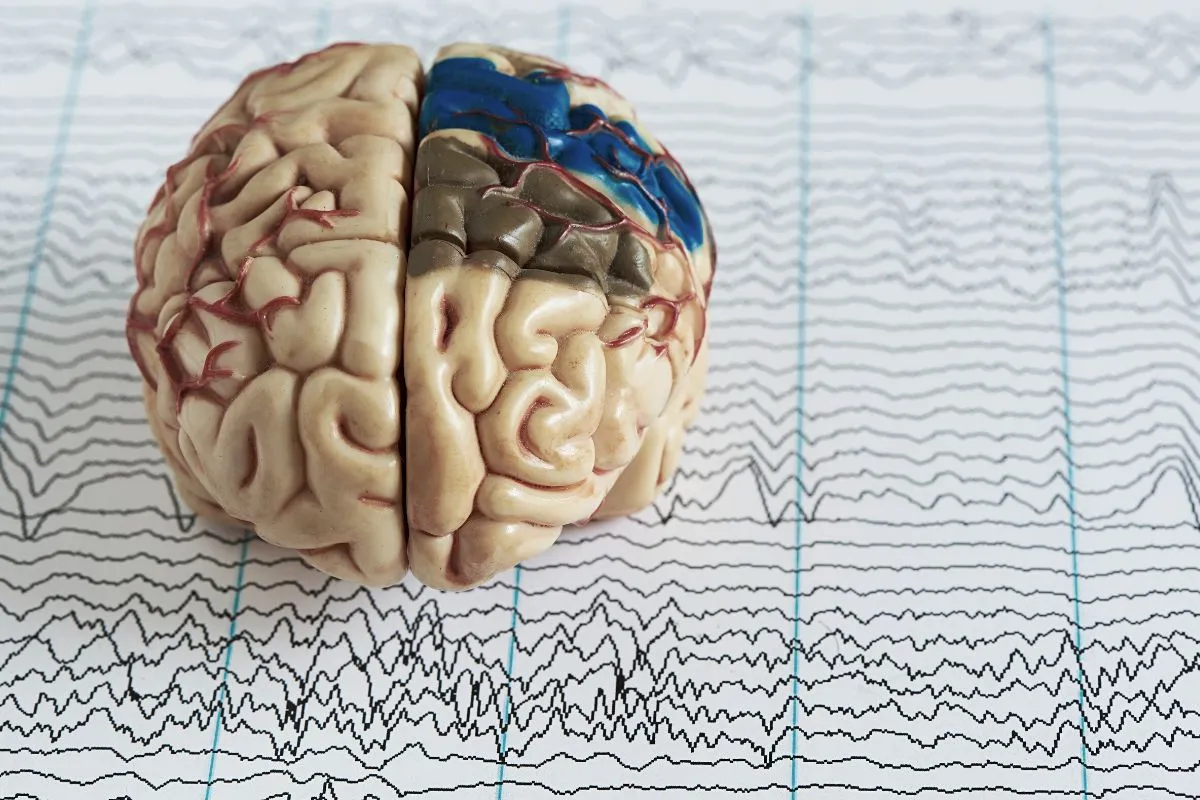
Diagnosing epilepsy
Diagnosis is primarily clinical, based on the patient’s history and eyewitness accounts. Some complementary tests help confirm the diagnosis and identify the cause:
Electroencephalogram (EEG): detects abnormal electrical patterns in the brain.
Magnetic resonance imaging (MRI): assesses possible structural brain lesions.
Computed tomography (CT scan): useful in cases of trauma or emergencies.
Treating epilepsy
Epilepsy is effectively treatable in most cases. The goal is to control seizures and allow the patient to live a normal life.
Antiepileptic medications
These are the main treatment and work by controlling abnormal brain activity. There are many options, and the choice of medication depends on the seizure type and individual characteristics. Continuous use under medical supervision is essential, as stopping treatment can trigger seizures.
Surgery
In cases of refractory epilepsy (when medications don’t control seizures), surgery may be performed to remove the brain area where seizures originate.
Vagus nerve stimulation and ketogenic diet
These are alternative treatments used in specific cases, especially for children or patients who do not respond well to conventional therapies.
Myths and facts about epilepsy
“All epileptic seizures are convulsions.”
❌ Myth. Not all seizures involve convulsions. Some may involve brief changes in behavior, speech, or awareness.
“Epilepsy is contagious.”
❌ Myth. Epilepsy is not contagious. It is a neurological condition, not an infection.
“People with epilepsy can’t live normal lives.”
❌ Myth. With proper treatment, many people with epilepsy live independently, work, study, and enjoy a good quality of life.
“It’s dangerous to put something in someone’s mouth during a seizure.”
✅ Fact. This can cause injury. The correct action is to turn the person on their side, protect their head, and wait for the seizure to pass.
“People with epilepsy can’t drive.”
✅ Partially true. Driving eligibility depends on seizure control, according to local laws. With proper management, many patients can return to driving.
Epilepsy in children and the elderly
Epilepsy can occur at any age, but it has two main peaks: in childhood and after age 60. In the elderly, it is often related to strokes or neurodegenerative diseases. In children, it may have genetic or unknown causes. In both groups, treatment is equally important and often effective.
When to seek help?
If you witness someone having a convulsive seizure for the first time, or if you are experiencing episodes of unconsciousness, involuntary movements, or memory lapses, seek medical attention. Early diagnosis and treatment of epilepsy are key to preventing complications and improving quality of life.