Atrial fibrillation (AF) is the most common cardiac arrhythmia globally, especially among people over the age of 60. It is characterized by irregular and often rapid heartbeats that can increase the risk of stroke, heart failure, and other serious complications.
Despite being frequent, atrial fibrillation doesn’t always cause noticeable symptoms, which means many cases are diagnosed late. In this article, we’ll take a closer look at what AF is, why it happens, how it’s diagnosed, and the available treatment options.
What is Atrial Fibrillation?
Atrial fibrillation is a type of arrhythmia in which the upper chambers of the heart (the atria) lose their ability to contract in a coordinated manner. Instead of beating regularly, the atria enter a fast and disorganized rhythm — as if they are “quivering” (fibrillating).
As a result, blood doesn’t circulate efficiently and may pool, forming clots. If a clot travels to the brain, it can cause an ischemic stroke.
Common Symptoms
The symptoms of atrial fibrillation can vary greatly. Some people don’t feel anything, while others experience intense symptoms. The most common include:
Palpitations (a sensation of a fast or “skipping” heartbeat)
Unexplained fatigue
Shortness of breath, especially during physical activity
Dizziness or near-fainting
Chest pain
Reduced exercise tolerance
It’s important to remember that AF can be asymptomatic, especially in older adults, and is often discovered incidentally during routine exams.
What Causes Atrial Fibrillation?
Atrial fibrillation can be triggered by a variety of conditions and is more common in people with:
High blood pressure (hypertension)
Coronary artery disease (such as prior heart attack)
Heart failure
Heart valve disease
Hyperthyroidism
Sleep apnea
Diabetes mellitus
Chronic lung disease
Other risk factors include aging, excessive alcohol consumption, obesity, and family history of AF.
Types of Atrial Fibrillation
AF can present in different forms:
Paroxysmal: episodes start and stop on their own, usually lasting less than 7 days
Persistent: episodes last more than 7 days and don’t resolve spontaneously
Long-standing persistent: AF lasting longer than one year
Permanent: when restoring normal rhythm is no longer pursued and the condition is accepted as ongoing
The type of AF influences treatment decisions.
Diagnosis
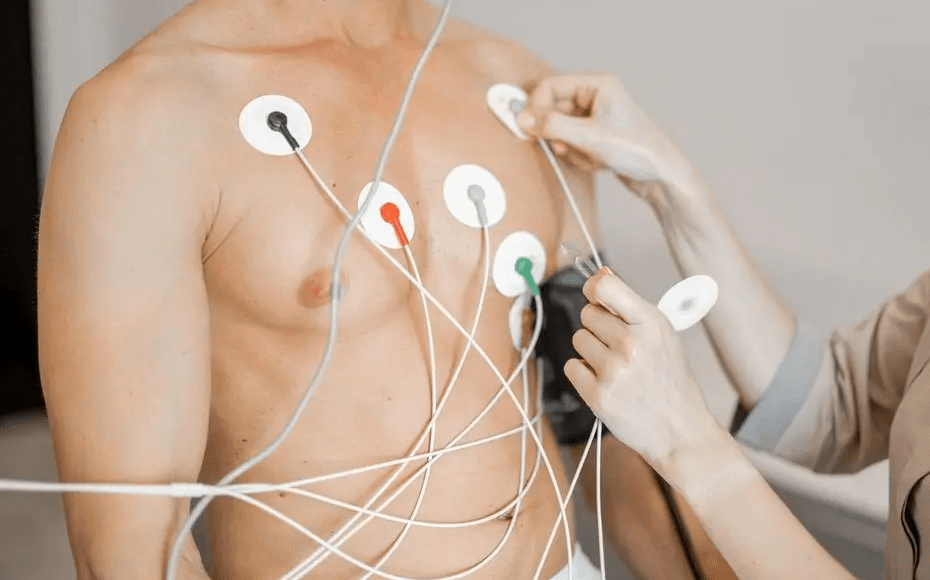
Diagnosis is based on tests that evaluate heart rhythm. The main ones include:
Electrocardiogram (ECG): detects the arrhythmia during the test
24-hour Holter monitor: records heart rhythm continuously for a day
Event monitor: worn over several days for intermittent symptoms
Echocardiogram: assesses heart structure and function
Laboratory tests: especially to check for hormonal or metabolic imbalances (e.g., thyroid function)
Risks of Atrial Fibrillation
The two greatest risks associated with AF are:
Stroke: clots formed in the atria can travel to the brain. It’s estimated that AF increases stroke risk by up to 5 times.
Heart failure: the loss of effective atrial contraction can impair heart function, eventually leading to heart failure.
AF is also linked to a higher risk of dementia and cardiovascular-related mortality.
Treatment: How to Manage Atrial Fibrillation
Treatment of AF generally focuses on three main goals:
1. Preventing Blood Clots
Anticoagulant therapy is essential in many cases to prevent stroke. Options include:
Warfarin (requires INR monitoring)
Direct oral anticoagulants (DOACs) such as rivaroxaban, apixaban, or dabigatran
The decision to use anticoagulants is based on risk scores like CHA₂DS₂-VASc.
2. Controlling Heart Rate
Certain medications help maintain a safe heart rate:
Beta-blockers (e.g., atenolol or metoprolol)
Calcium channel blockers (verapamil, diltiazem)
Digoxin (in specific cases)
3. Restoring Normal Sinus Rhythm
For some patients, it’s possible to try restoring the heart’s normal rhythm using:
Electrical cardioversion (controlled shock to reset rhythm)
Antiarrhythmic medications (e.g., amiodarone)
Catheter ablation: a procedure that destroys arrhythmia-causing areas in the heart
The choice between rate control and rhythm control depends on several factors such as age, AF duration, and symptom severity.
Living with Atrial Fibrillation
While AF often has no definitive cure, it can be effectively managed with proper treatment and regular medical follow-up.
Lifestyle changes can also make a big difference:
Keep blood pressure and cholesterol under control
Treat sleep apnea if present
Limit alcohol intake
Maintain a healthy weight
Engage in moderate physical activity (with medical guidance)
You can also explore our free health calculators to support lifestyle management:
Conclusion
Atrial fibrillation is a common and potentially dangerous condition, but it can be managed with the right treatment and healthy habits. Being aware of the symptoms — or lack thereof — is essential, especially in older adults or those with heart conditions.
If you or someone close to you has a history of AF, don’t hesitate to consult a cardiologist and maintain regular checkups. Early diagnosis and the prevention of complications can save lives.