Content covered in this post
What Huntington’s disease is
Symptoms: motor, cognitive, and behavioral
Causes and heredity (HTT/CAG)
Diagnosis and key differentials
Treatment and multidisciplinary care
Lifestyle and safety
Research and advances
Quick FAQ
Health disclaimer
How VirtualCare can help
References & recommended reading (last item)
What is Huntington’s disease?
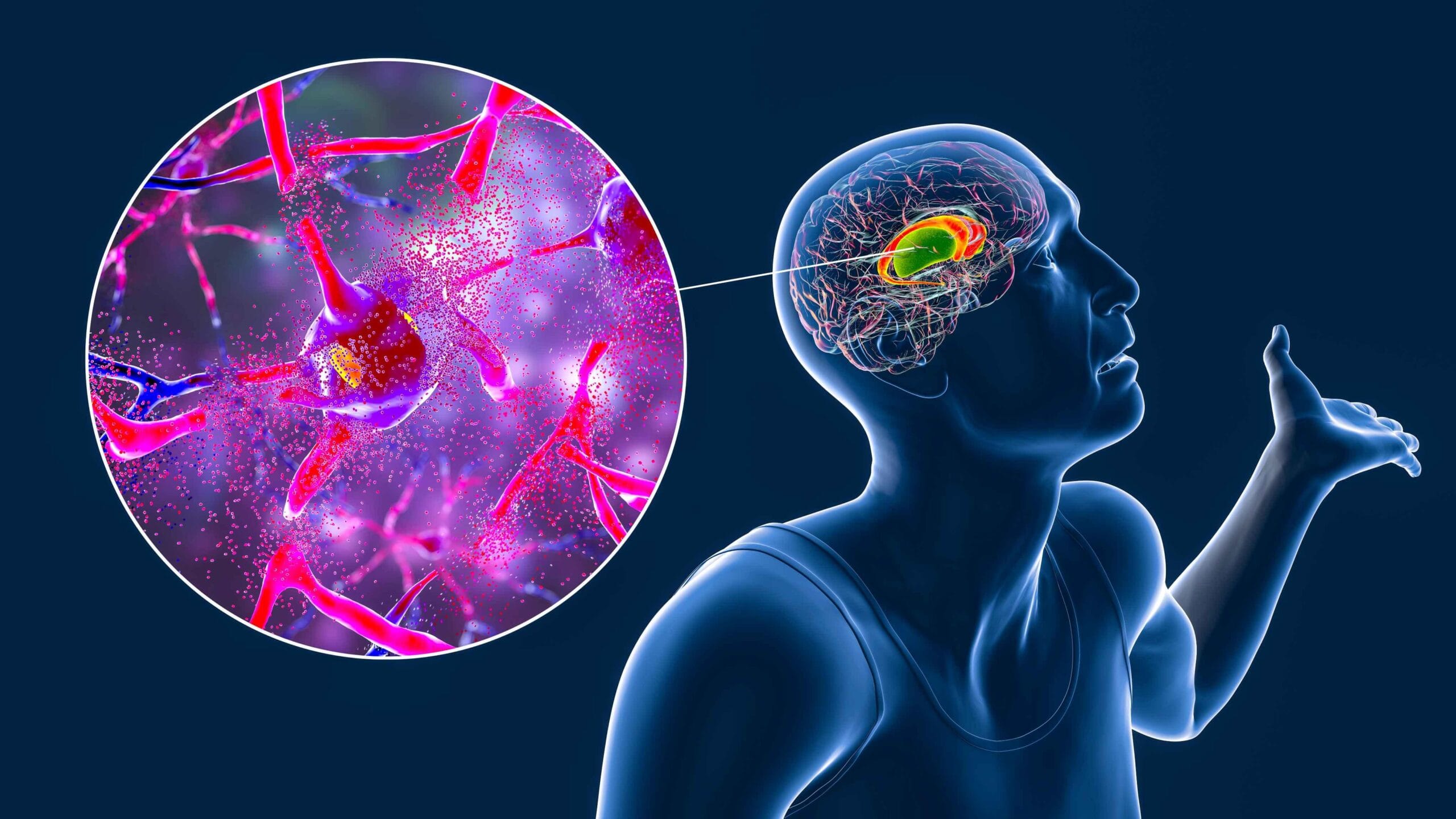
Huntington’s disease (HD) is a genetic condition that leads to progressive degeneration of neurons, especially in the striatum. Onset typically occurs between ages 30–50, but it can appear before age 20 (juvenile-onset HD). Progression is gradual; average life expectancy after symptom onset is ~15–20 years, with wide individual variation.
Why it matters: HD combines involuntary movements (chorea), cognitive changes (executive function, attention, memory), and behavioral symptoms (depression, irritability), affecting patients, families, and caregivers. With continuous, team-based care, risks like falls, aspiration, malnutrition, and psychological distress can be reduced.
Symptoms: motor, cognitive, and behavioral
Motor
Chorea (hallmark): rapid, irregular, involuntary movements
Rigidity, dystonia, gait changes; postural instability and falls
Dysarthria (slurred speech) and dysphagia (swallowing difficulty)
Cognitive
Slowed thinking and executive dysfunction (planning, organization, decision-making)
Progressive attention and memory difficulties
Behavioral/psychiatric
Irritability, anxiety, depression, apathy
Disinhibition, personality changes; psychosis in some cases
Juvenile-onset HD (<20 years) often shows less chorea and more rigidity, seizures, and faster progression.
Causes and heredity (HTT/CAG)
Caused by an expanded CAG repeat in the HTT gene → toxic, mutant huntingtin protein
Autosomal dominant inheritance: one altered copy is enough
Risk to children: 50% per pregnancy
Repeat length: larger CAG expansions are associated with earlier onset (not an absolute rule)
Predictive testing: available to asymptomatic adults; must include genetic counseling and psychological support
Family planning: discuss preimplantation genetic testing (PGT) and options with a specialized team
Diagnosis and differentials
Diagnosis combines clinical and family history, neurological exam, and genetic testing confirming CAG expansion in HTT.
Supportive assessments
Brain MRI may show caudate/striatal atrophy in later stages
Neuropsychological evaluation to profile cognitive changes
Swallowing and nutrition evaluations to assess aspiration and weight-loss risks
Key differentials
Other choreas (autoimmune, drug-induced, thyroid-related)
Atypical parkinsonian syndromes
Frontotemporal dementias
Treatment and multidisciplinary care
There is no cure yet, but treatment can markedly reduce symptoms and improve quality of life.
Motor symptom control
VMAT2 inhibitors: tetrabenazine and deutetrabenazine can reduce chorea
Atypical antipsychotics (e.g., risperidone, olanzapine) may help with chorea and behavioral symptoms
Monitor for sedation, parkinsonism, metabolic effects
Mental health
SSRIs for depression/anxiety; ongoing psychotherapy and psychosocial support
Proactive monitoring for suicidal ideation
Rehabilitation & nutrition
Physical therapy (physiotherapy): gait/balance training, fall prevention
Occupational therapy: home/adaptive equipment to maximize independence
Speech-language pathology (SLP): swallowing safety and communication strategies
Nutrition: higher-calorie, frequent meals; supplements as needed; dysphagia precautions
Planning & safety
Regular medication reviews to minimize interactions and iatrogenesis
Environmental adaptations (grab bars, non-slip rugs, good lighting)
Advance care planning/advance directives while decision-making capacity is preserved
Caregiver support: education, respite resources, and burnout prevention
Lifestyle and safety
Structured routines with visual reminders; break tasks into simple steps
Tailored physical activity (light aerobic + strengthening) as advised by your care team
Sleep hygiene (morning light exposure, limit caffeine late day)
Social engagement and meaningful activities for well-being and cognitive stimulation
Research and advances
Active research areas include:
Gene silencing (antisense oligonucleotides, RNA interference) to lower mutant huntingtin
Protein homeostasis/modulation to reduce cellular toxicity
Gene editing (pre-clinical) and biomarkers (blood/CSF) to track therapeutic response
Results vary across trials. Discuss eligibility and expectations with experienced centers; participation depends on individual factors and study criteria. Availability of therapies and trials differs by country.
Quick FAQ
1) Is it contagious?
No. HD is hereditary due to a genetic mutation.
2) Are my children at risk?
If you carry the mutation, each child has a 50% risk. Seek genetic counseling.
3) Should I get predictive testing?
A personal, complex decision. Always include pre-/post-test genetic counseling and psychological support.
4) Is juvenile-onset HD different?
Usually begins before age 20, progresses faster, with more rigidity and possible seizures.
Important notice (health disclaimer)
This content is educational and does not replace medical care. For diagnosis and individualized treatment, consult a qualified healthcare professional in your region.
References & recommended reading
GeneReviews® — Huntington Disease. University of Washington, Seattle.
NINDS — Huntington’s Disease. National Institute of Neurological Disorders and Stroke (NIH).
Bates GP, et al. Huntington disease. Nat Rev Dis Primers. 2015;1:15005.
Tabrizi SJ, et al. Targeting Huntingtin Expression in Patients with Huntington’s Disease. N Engl J Med. 2019;380:2307–2316.
American Academy of Neurology (AAN). Evidence-based guideline update: Pharmacologic treatment of chorea in Huntington disease.
European Huntington Disease Network (EHDN). Physiotherapy/Multidisciplinary care recommendations.
Ross CA, et al. Huntington disease: natural history, biomarkers and prospects for therapeutics. Mov Disord. 2014.