Content discussed in this post
What sickle cell disease is
Symptoms and how the disease presents across the lifespan
Complications that require immediate attention
Sickle cell trait vs sickle cell disease
Diagnosis, newborn screening, and tests
Day-to-day treatment and infection prevention
Vaso-occlusive crises: what to do
Transfusions, iron overload, and monitoring
Transplant and gene therapy: where we are
Lifestyle, sports, travel, and pregnancy
Quick FAQ
Important notice (health disclaimer)
References and recommended reading
What sickle cell disease is
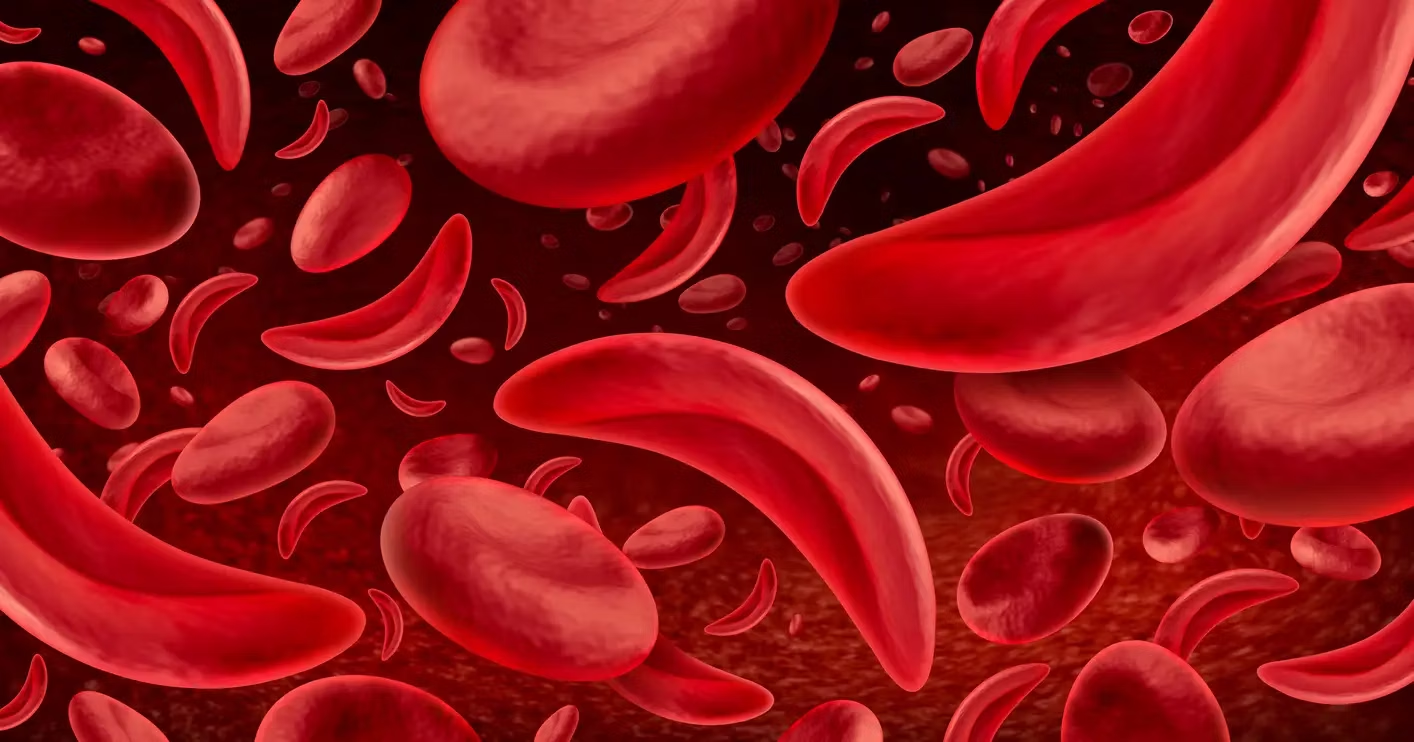
Sickle cell disease is an autosomal recessive genetic condition. A change in the beta-globin gene leads to production of hemoglobin S (HbS). In low-oxygen states, dehydration, or fever, HbS polymerizes, deforming red blood cells into a sickle shape. These cells become rigid, break more easily (hemolysis), and block small blood vessels (vaso-occlusion). The result is chronic anemia, pain, and risk of organ damage.
Symptoms and how the disease presents across the lifespan
Early signs can appear in infancy. Babies have partial protection from fetal hemoglobin, so manifestations increase after 4 to 6 months.
Pain crises (hands and feet in childhood, later long bones, back, chest)
Anemia with jaundice, fatigue, and pallor
More severe infections, especially from encapsulated bacteria, due to progressive loss of splenic function
Delays in growth and puberty in more symptomatic cases
Chronic complications vary: leg ulcers, chronic pain, renal changes, retinopathy, avascular necrosis of the femoral head, priapism.
Complications that require immediate attention
Acute chest syndrome: chest pain, shortness of breath, fever, and oxygen desaturation. It can resemble pneumonia and is a leading cause of hospitalization.
Splenic sequestration (especially in children): sudden splenic enlargement, marked pallor, and sharp hemoglobin drop. This is an emergency.
Stroke: higher risk in childhood and adolescence. Sudden neurological signs require urgent care.
Febrile infection: fever in someone with sickle cell disease always warrants prompt evaluation.
Prolonged priapism: painful erection lasting more than 4 hours requires immediate care.
Sickle cell trait vs sickle cell disease
Those who inherit one HbS gene and one normal gene have sickle cell trait. They are generally asymptomatic and do not progress like the disease. Those who inherit two altered genes (HbSS) or combinations with other variants (HbSC, Sβ-thalassemia) have sickle cell disease, with clinical manifestations. Trait status matters for genetic counseling and in specific contexts of extreme low oxygen, severe dehydration, or high altitude.
Diagnosis, newborn screening, and tests
Newborn screening identifies the condition early in many countries.
Hemoglobin electrophoresis or HPLC confirms hemoglobin type.
Routine labs assess hemoglobin, reticulocytes, bilirubin, renal and liver function.
In childhood, annual transcranial Doppler helps measure stroke risk and guide prevention.
Day-to-day treatment and infection prevention
Hydroxyurea increases fetal hemoglobin, reduces crises and hospitalizations. It is a mainstay for many patients.
Folic acid supplementation supports red cell production.
Penicillin prophylaxis in childhood and vaccination are essential: pneumococcal (PCV and PPSV as per schedule), Haemophilus influenzae type b, meningococcal, annual influenza, and routine immunizations.
Hydration, avoiding temperature extremes, early treatment of infections, and regular follow-up with hematology make a long-term difference.
Vaso-occlusive crises: what to do
During a crisis, prioritize adequate analgesia, hydration, gentle warming, and investigation of triggers such as infections. In selected cases, oxygen therapy, antibiotics, and hospitalization may be necessary. Written management plans, agreed upon with the care team, help decide when to go to the hospital.
Transfusions, iron overload, and monitoring
Simple transfusion or exchange transfusion is used in specific scenarios: stroke prevention in high-risk children, severe acute chest syndrome, surgical preparation, or very symptomatic anemia.
Iron overload can occur with repeated transfusions. Monitoring includes ferritin, and iron chelators are used when needed.
Transplant and gene therapy: where we are
Hematopoietic stem cell transplant can cure the disease in a subset of cases, especially with a compatible donor and in experienced centers.
Gene therapies have begun to reach practice in some countries, either by reducing expression of genes that suppress fetal hemoglobin or by introducing a functional version of beta-globin. These are promising technologies with indications for specific profiles and require close safety and efficacy follow-up. Discuss eligibility, risks, and regional access with the team.
Lifestyle, sports, travel, and pregnancy
Physical activity is welcome with hydration, breaks, and temperature adaptation.
Travel: plan hydration, avoid hypoxia (very high altitudes or inadequately pressurized cabins), and carry medical documentation.
Pregnancy: requires high-risk care. The disease increases the chances of maternal and fetal complications. Preconception planning and coordination between obstetrics and hematology are essential.
Mental health and chronic pain: psychological support, physical therapy, relaxation techniques, and pain teams help with comprehensive management.
Quick FAQ
Is sickle cell disease curable?
Cure is possible for some through transplant and, in selected settings, emerging gene therapies. For many people the focus is reducing crises and protecting organs over a lifetime.
Is hydroxyurea safe?
For most patients, yes, with periodic monitoring. It reduces crises and the need for hospitalization.
Is every fever an emergency?
Fever warrants rapid evaluation. People with sickle cell disease are at higher risk of severe infections.
Can I donate my own blood in advance to avoid transfusions?
Autologous donation does not address the typical acute situations. Transfusion decisions are medical and individualized.
Does sickle cell trait cause symptoms?
In most people, no. It matters for genetic counseling and in some extreme contexts.
Important notice (health disclaimer)
This content is educational and does not replace medical care. Management of sickle cell disease must be individualized, with regular follow-up and an action plan for crises and travel. In cases of fever, severe pain, or shortness of breath, seek immediate care.
References and recommended reading
WHO / PAHO. Sickle cell disease: key facts and management guides.
NIH / NHLBI. Evidence-based management of sickle cell disease.
ASH Guidelines. Recommendations on hydroxyurea, transfusion, and stroke prevention.
Cochrane Reviews. Interventions for sickle cell disease: hydroxyurea, transfusion, iron chelators.
CDC. Newborn screening, vaccination schedules, and travel counseling.
AABB. Transfusion best practices in sickle cell disease.
Recent publications on transplant and gene therapy from reference centers.