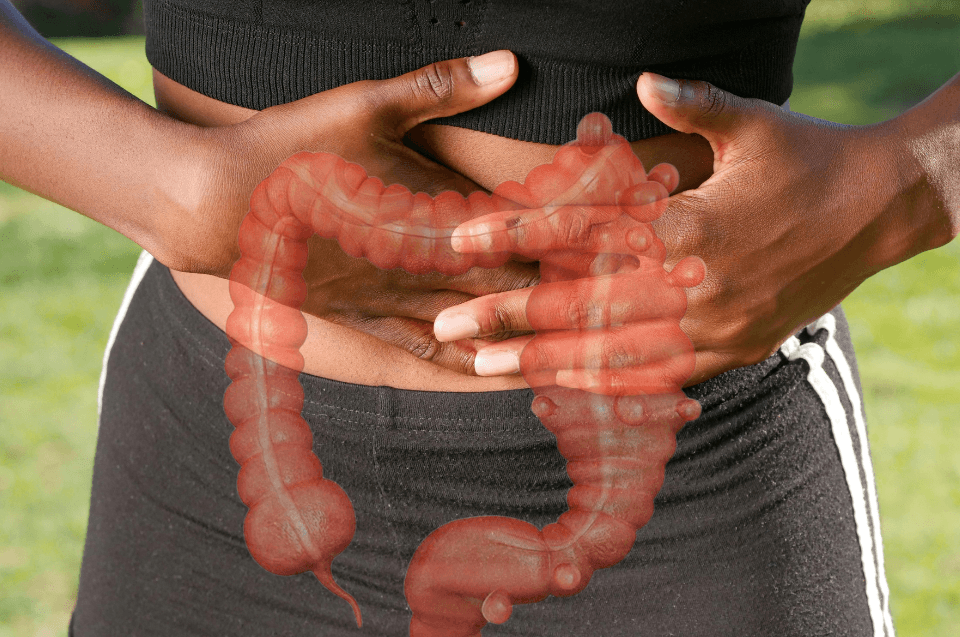
Diverticulitis is a condition that occurs when small pouches that form in the wall of the large intestine, called diverticula, become inflamed or infected. It is relatively common, especially in people over the age of 40, and can range from mild cases to severe ones requiring hospitalization.
Although often confused with diverticulosis — the presence of diverticula without inflammation — diverticulitis is the more serious form and can lead to complications such as abscesses and intestinal perforation.
What Causes Diverticulitis?
The exact cause is not fully understood, but inflammation is believed to occur when stool or bacteria become trapped inside the diverticula. Key risk factors include:
Age: more frequent after age 40.
Low-fiber diet: increases the risk of diverticula formation.
Sedentary lifestyle: lack of exercise is linked to higher risk.
Obesity: excess weight favors development of the disease.
Certain medications: such as NSAIDs, corticosteroids, and opioids.
Family history: having close relatives with the condition raises the risk.
Symptoms of Diverticulitis
Symptoms vary from person to person but often include:
Abdominal pain, usually in the lower left side
Fever
Nausea and vomiting
Bowel habit changes (constipation or diarrhea)
Abdominal tenderness to touch
Bloating
In more severe cases, complications may occur, such as abscesses, intestinal perforation, peritonitis, or bowel obstruction.
Diagnosis
Diagnosis involves both clinical evaluation and imaging tests. Common exams include:
Blood tests: to check for signs of infection.
Abdominal CT scan: considered the gold standard for confirming diagnosis and identifying complications.
Ultrasound: may be useful in some patients, especially younger individuals or pregnant women.
Colonoscopy, while important in assessing the colon for other conditions, is generally avoided during acute diverticulitis due to the risk of perforation.
Treatment for Diverticulitis
Treatment depends on the severity of the case:
Mild cases: often managed at home with temporary liquid diet, oral antibiotics, and pain relief.
Moderate to severe cases: usually require hospitalization, intravenous antibiotics, hydration, and close monitoring.
Complicated cases: such as abscesses or perforation, may require surgical drainage or resection of part of the intestine.
After recovery from the acute phase, patients may need lifestyle adjustments to reduce the risk of recurrence.
Prevention
Prevention is closely tied to diet and lifestyle. Effective measures include:
Eating more fiber: fruits, vegetables, legumes, and whole grains help regulate bowel movements.
Staying hydrated: drinking enough water prevents constipation.
Exercising regularly: improves intestinal motility.
Maintaining a healthy weight: reduces risk of flare-ups.
Avoiding excessive use of NSAIDs without medical supervision.
Myths, Facts, and Scientific Advances
Myth: People with diverticula should avoid seeds, corn, or popcorn, as they might “block” diverticula.
Fact: Research shows no scientific evidence supporting this restriction.Curiosity: Diverticulitis is more common in Western countries, likely due to low-fiber diets and sedentary lifestyles.
Scientific advance: New research suggests the gut microbiota may play a role in diverticulitis, with imbalances in intestinal bacteria potentially influencing inflammation risk.
Final Considerations
Diverticulitis can range from mild to severe, but with early diagnosis and proper treatment, most patients recover without major complications. A fiber-rich diet, regular physical activity, and medical follow-up are essential to lower the risk of recurrence and improve quality of life.
Seeking immediate medical care when experiencing symptoms such as severe abdominal pain and fever is critical to prevent serious complications.