Contents covered in this post
What cirrhosis is and how it develops
Leading causes today
Signs and symptoms
How the diagnosis is made
Staging and prognosis
Complications of portal hypertension
Hepatic encephalopathy
Liver cancer risk and surveillance
Treatment and management
Lifestyle, vaccination, and prevention
When to seek medical care
Quick FAQ
Important notice (health disclaimer)
References and recommended reading
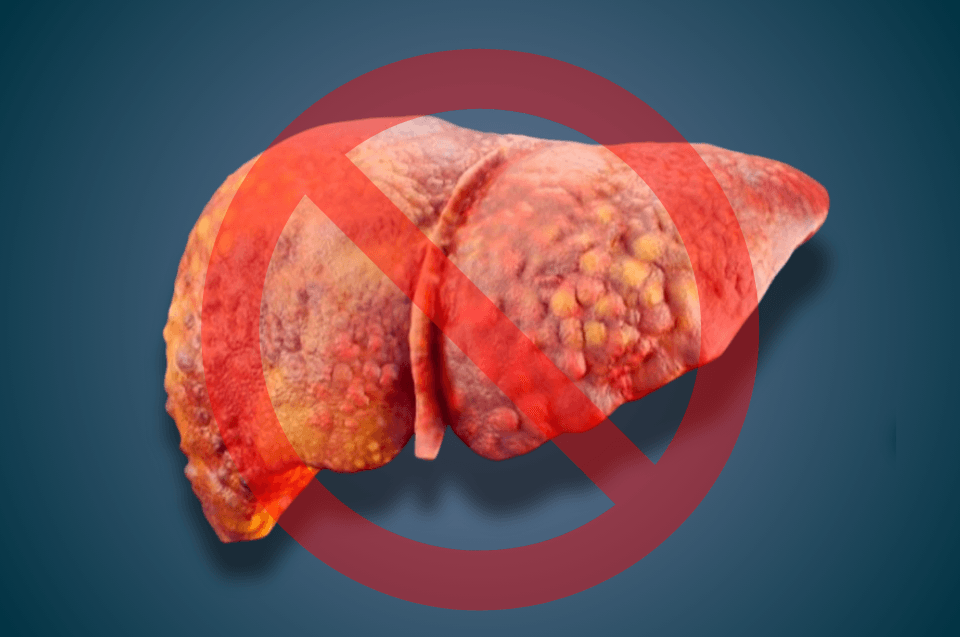
What cirrhosis is and how it develops
Cirrhosis is the advanced stage of liver fibrosis caused by chronic inflammation. Repeated injury triggers scar formation and architectural remodeling with regenerative nodules and portal hypertension. The liver progressively loses key functions such as protein synthesis, detoxification, and regulation of coagulation and glucose. The disease may remain compensated for years, then become decompensated when complications like ascites, variceal bleeding, encephalopathy, or jaundice appear.
Leading causes today
Causes vary by region, but globally the main drivers are:
Harmful alcohol use and alcohol use disorder
Chronic viral hepatitis B and C, with a declining impact where diagnosis and treatment are widespread
Metabolic dysfunction–associated steatohepatitis (MASH, previously NASH), related to obesity, insulin resistance, diabetes, and dyslipidemia
Less common causes: autoimmune cholangiopathies, hemochromatosis, Wilson disease, autoimmune hepatitis, chronic biliary obstruction, and hepatotoxic drugs
Identifying the underlying cause guides treatment and can slow progression.
Signs and symptoms
Compensated disease may be silent. Over time, people can develop:
Fatigue, loss of appetite, loss of muscle mass
Jaundice, dark urine, pale stools
Itching, easy bruising, leg edema
Ascites with abdominal distension
Cognitive slowing, daytime sleepiness, sleep–wake inversion due to hepatic encephalopathy
In advanced cases: marked weakness, hyponatremia, recurrent infections
How the diagnosis is made
Diagnosis combines clinical assessment, labs, and imaging:
Blood tests: liver enzymes, bilirubin, albumin, INR, platelets
Abdominal ultrasound for signs of portal hypertension and parenchymal changes
Liver elastography (transient or MR-based) to estimate stiffness and fibrosis without biopsy
Upper endoscopy to screen for varices in people with cirrhosis
Liver biopsy when the diagnosis is uncertain or to clarify etiology
Etiologic work-up: hepatitis B and C serologies, autoimmune panel, iron studies and ferritin, ceruloplasmin, and metabolic profile as indicated
Staging and prognosis
Two systems are commonly used:
Child-Pugh: bilirubin, albumin, INR, ascites, encephalopathy. Classes A, B, or C reflect severity.
MELD: continuous score based on bilirubin, INR, creatinine, and sodium. Used for transplant prioritization and risk estimation.
Clinically, distinguishing compensated from decompensated cirrhosis is key. The first decompensation changes prognosis and follow-up intensity.
Complications of portal hypertension
Elevated portal pressure leads to:
Esophagogastric varices: bleeding risk. Primary prophylaxis with a nonselective beta-blocker or endoscopic band ligation in high-risk varices. Acute bleeding requires coordinated management with resuscitation, vasoactive agents, antibiotics, and therapeutic endoscopy.
Ascites: manage with moderate salt restriction, diuretics, and large-volume paracentesis when tense. Evaluate for spontaneous bacterial peritonitis with any clinical worsening.
Hepatorenal syndrome: kidney dysfunction in advanced cirrhosis with splanchnic vasodilation that needs specific therapy.
Hypersplenism: thrombocytopenia from splenic sequestration.
Hepatic encephalopathy
A brain dysfunction due to accumulated toxins not cleared by the liver. Severity ranges from subtle attention deficits to coma. Management includes:
Lactulose to reduce ammonia absorption and promote bowel movements
Rifaximin as an add-on for recurrent episodes
Correcting triggers such as infection, constipation, bleeding, sedatives, hypokalemia, and dehydration
Patients and families should recognize early signs like confusion, inattention, unusual sleepiness, and disorientation.
Liver cancer risk and surveillance
Cirrhosis of any cause increases the risk of hepatocellular carcinoma (HCC). Recommendations:
Semiannual ultrasound of the liver, with or without alpha-fetoprotein (AFP), for early detection
Suspicious lesions need multiphase contrast-enhanced MRI or CT using established radiologic criteria
Early diagnosis enables potentially curative options for selected patients such as ablation, surgical resection, or transplantation
Treatment and management
Care combines treating the cause, preventing and managing complications, and evaluating for transplant when appropriate.
Treat the cause
Alcohol: complete abstinence, multidisciplinary support, and treatment for alcohol use disorder
Hepatitis B: antivirals with a high barrier to resistance
Hepatitis C: direct-acting antivirals with high cure rates
MASH: gradual weight loss, metabolic control, physical activity, and evaluation of approved pharmacotherapy where available
Autoimmune and cholestatic diseases: immunosuppressants and ursodeoxycholic acid according to guidelines
Manage complications
Ascites: diuretics; large-volume paracentesis with albumin when indicated; evaluate TIPS in selected cases
Varices: primary and secondary prophylaxis, and standard algorithms for acute bleeding
Encephalopathy: lactulose, rifaximin, and trigger correction
Infections: heightened vigilance, scenario-specific prophylaxis, and early treatment
Liver transplantation
Indicated for decompensated cirrhosis with high MELD or recurrent complications, and for HCC within transplant criteria. Early referral improves outcomes.
Patient education is central: recognize decompensation, adhere to medications, attend surveillance imaging and endoscopy, and keep vaccinations up to date.
Lifestyle, vaccination, and prevention
Alcohol abstinence is pivotal whenever alcohol contributes to disease
Nutrition: adequate protein intake, meal spacing, and a bedtime protein snack if sarcopenia is present. Avoid unnecessary restrictions without professional guidance
Vaccines: hepatitis A and B if susceptible, annual influenza, pneumococcal per age and risk, and routine updates
Avoid common NSAIDs and unverified herbal products without medical advice
Metabolic health: address weight, glucose, blood pressure, and lipids
When to seek medical care
Seek urgent evaluation for:
Rapid abdominal enlargement, severe pain, persistent vomiting, or fever
Vomiting blood or black stools
Confusion, excessive sleepiness, or fine tremors
Worsening jaundice, intense itching, very dark urine
Reduced urine output, dizziness, or hypotension
These are signs of decompensation that require prompt care.
Quick FAQ
Is cirrhosis curable?
Advanced fibrosis can stabilize and sometimes partially regress if the cause is controlled. In decompensated disease, transplant is the curative option.
Can people with cirrhosis eat normal amounts of protein?
Yes. Routine protein restriction is not recommended. Adjustments are individualized, including in encephalopathy.
What can I take for pain?
Avoid NSAIDs. Acetaminophen/paracetamol within safe dosing may be used short term with medical guidance.
If I cured hepatitis C, do I still need liver cancer surveillance?
Yes, if cirrhosis is present. HCC risk falls but does not go to zero.
Important notice (health disclaimer)
This content is educational and does not replace medical care. Cirrhosis management is individualized and requires a multidisciplinary team, a plan for complications, and periodic assessment for transplant when indicated.
References and recommended reading
AASLD. Practice guidance on cirrhosis: diagnosis, management, and complications.
EASL. Clinical practice guidelines on decompensated cirrhosis and portal hypertension.
WHO. Frameworks for prevention, testing, and treatment of hepatitis B and C.
APASL. Recommendations on variceal bleeding, ascites, and encephalopathy.
Cochrane Reviews. Interventions for hepatic encephalopathy, ascites, and prophylaxis in cirrhosis.
National hepatology societies. Country-specific guidelines for cirrhosis and its complications.